Mesothelioma is a cancer often linked to asbestos exposure. While treatments exist, they’re rarely curative. Scientists are now focusing on a surprising player in this disease: macrophages, a type of immune cell that normally protects the body. This blog explains how these cells accidentally fuel mesothelioma— nd how new therapies could turn them into cancer fighters.
Asbestos, Inflammation, and the Start of Trouble
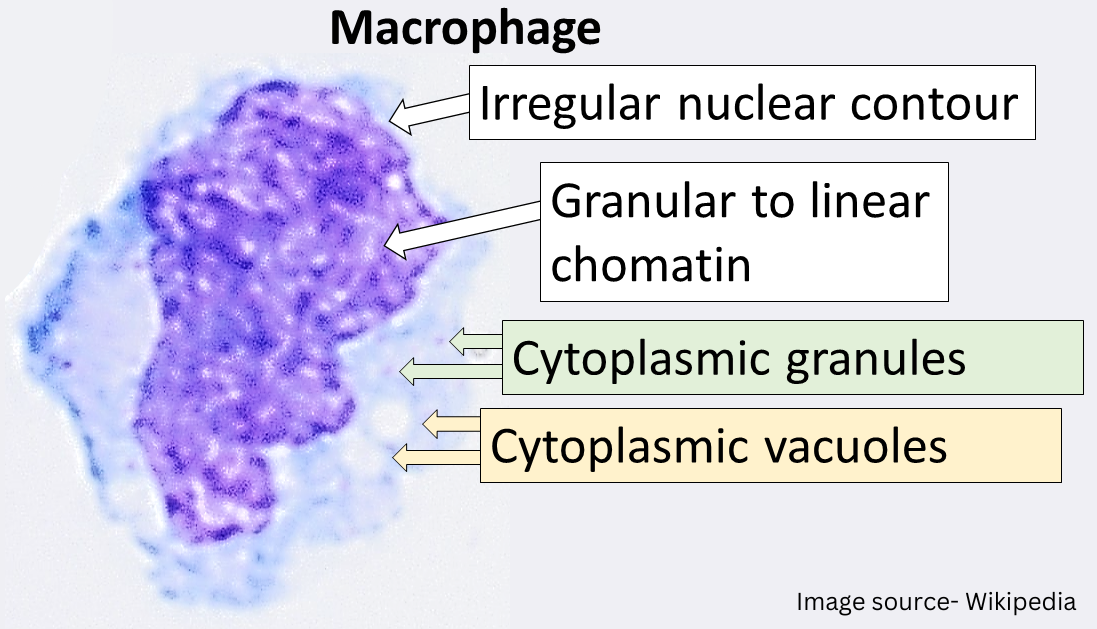
When asbestos fibers are inhaled, they stick in the lungs’ protective lining (pleura). The body sends macrophages—the immune system’s “cleanup crew”—to remove these fibers. But asbestos is tough to break down, so macrophages get stuck trying. This leads to long-term inflammation, which damages healthy cells over time and can trigger cancer.
What Science Tells Us:
- Asbestos causes macrophages to release harmful signals (like IL-1β and ROS) that damage nearby tissues.
- Chronic inflammation from failed cleanup efforts creates a perfect environment for cancer to develop.
When Helpers Become Harmful: The Role of Tumor-Associated Macrophages
Once mesothelioma forms, the tumor hijacks macrophages, turning them into tumor-associated macrophages (TAMs). Instead of fighting cancer, these TAMs become the tumor’s allies.
Also Read: 7 Daily Habits to Manage Mesothelioma Symptoms
How TAMs Help Cancer Grow:
- Silencing the Immune System: TAMs release signals that weaken other immune cells (like T cells), making it harder for the body to attack the tumor.
- Feeding the Tumor: TAMs help tumors grow new blood vessels, supplying them with oxygen and nutrients.
- Spreading Cancer: TAMs produce enzymes that break down tissue barriers, helping cancer cells spread to other organs.
Key Finding: Studies show that patients with high levels of TAMs in their tumors often have worse outcomes.
Current Treatments and Why We Need Better Options
Standard treatments like surgery, chemotherapy, and radiation can slow mesothelioma but rarely cure it. Immunotherapies (drugs that boost the immune system) work for some patients, but not all. This is why scientists are excited about targeting TAMs—it could help existing treatments work better.
New Treatments Targeting Macrophages
Researchers are testing therapies to reprogram TAMs or stop them from helping tumors. Here are three promising approaches:
Also Read: Can Mesothelioma Go Into Remission?
1. Blocking the “Survival Signal” for Harmful Macrophages
- How It Works: Drugs like CSF-1R inhibitors block a protein that TAMs need to survive. Fewer TAMs mean less support for the tumor.
- Progress: Early trials combining these drugs with chemotherapy have shown improved results in mesothelioma patients.
2. Activating Macrophages to Fight Cancer
- How It Works: Drugs called CD40 agonists “switch on” macrophages, turning them back into cancer fighters.
- Progress: Early studies in cancers like mesothelioma show tumors shrinking when these drugs are used.
3. Supercharging Macrophages with Gene Therapy
- How It Works: Scientists are engineering macrophages in the lab to recognize and attack cancer cells, then infusing them into patients (called CAR-M therapy).
- Potential: Lab tests show these modified macrophages can kill mesothelioma cells. Human trials are next.
Challenges and Hope for the Future
While these therapies are exciting, challenges remain. Mesothelioma varies between patients, so treatments may not work for everyone. There’s also a risk of side effects, like excessive inflammation. However, institutions like the National Cancer Institute (NCI) and top cancer centers are prioritizing research to address these issues.
What This Means for Patients
Understanding the role of macrophages opens doors to smarter, more personalized treatments. For example, a patient with high TAM levels in their tumor might benefit most from CSF-1R inhibitors. Clinical trials are critical to advancing these options, and patients in the U.S. can ask their doctors about joining studies.
Also Read: The History of Asbestos Use and Its Link to Mesothelioma
Conclusion
Macrophages are a double-edged sword in mesothelioma: they start as the body’s firefighters but end up fueling the cancer. However, new therapies aim to tip the balance back in the patient’s favor. While more research is needed, these advances offer real hope for better outcomes.
This blog provides general information about mesothelioma and emerging treatments. Always consult your doctor or sources like the American Cancer Society or National Cancer Institute for advice tailored to your health.
2 thoughts on “How Macrophages Fuel Mesothelioma Growth and Offer New Treatment Hopes”